Recently updated on October 30th, 2023 at 09:57 am
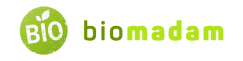
Crohn’s disease and ulcerative colitis are diseases of the gastrointestinal tract relating to inflammatory bowel syndrome. Crohn’s disease may affect the whole gastrointestinal tract, while ulcerative colitis is the inflammation of the colon. These diseases have similar symptoms, so even diagnosis and prognosis seem similar at times. They typically develop in young adults and teens. However, they can develop at other ages too. Let’s tell you the differences between Crohn’s disease and ulcerative colitis in detail.
Comparison Table
| Characteristics | Crohn’s Disease | Ulcerative Colitis |
| Definition | Inflammation of GI tract | Inflammation of colon |
| Genetic Risk | Higher | Lower |
| Area of Inflammation | Anywhere from mouth to anus | Colon |
| Extent of Inflammation | Intermittent | Continuous |
| Classification | Ileitis, gastroduodenal, jejunoileitis, and ileocolitis | Proctitis, proctosigmoiditis, left-sided colitis, and pancolitis |
| Symptoms | Diarrhea, fever, fatigue, blood in stools, sores, etc. | Sore throat, weight loss, blood in stools, back pain |
| Causes | Genetic variables, smoking environmental factors, IBD | Genetics, autoimmune reactions, external factors |
| Diagnosis | Colonoscopy, endoscopy | Sigmoidoscopy, colonoscopy |
| Treatment | Dietary changes, medicines | Drugs, and surgery |
| Surgery | Rare | Common |
What is Crohn’s Disease?
Crohn’s disease is a subtype of IBD, inflammatory bowel disease. It causes inflammation (swelling) of the tissues in the digestive tract, which can lead to abdominal pain, severe diarrhea, exhaustion, weight loss, and malnutrition. Crohn’s disease is both inflammatory and autoimmune.
Crohn’s disease affects the gastrointestinal tract, from mouth to anus, but typically strikes between the terminal ileum and the first part of the colon. It can influence the thickness of the wall of the intestine. Intestinal inflammation can skip or leave healthy tissue between diseased areas.
Younger people risk developing Crohn’s disease more than older people. Nonetheless, this issue can arise at any time in life. The condition affects both men and women equally. Crohn’s disease also manifests in infants and toddlers. Smoking cigarettes may increase your risk of Crohn’s disease by affecting your lungs.
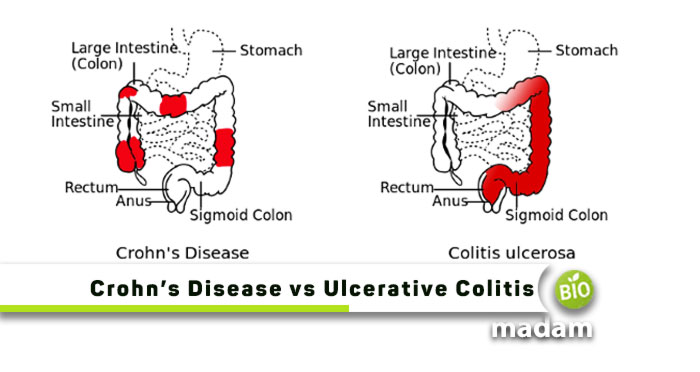
Symptoms of Crohn’s Disease
Variation in Crohn’s disease among patients is common. The symptoms of Crohn’s disease can be excruciating, debilitating, and sometimes life-threatening. The symptoms tend to fluctuate between active phases, known as flares, and remission phases, during which you may not experience any signs and symptoms.
Crohn’s disease can affect the entire gastrointestinal tract, from the mouth to the anus. Inflammation of the GI tract due to Crohn’s disease manifests in various ways, but some symptoms are common. They include:
- Ongoing diarrhea
- Rectal hemorrhage
- Urgent need to defecate
- Abdominal discomfort and cramps
- Constipation, which can lead to bowel obstruction (potentially life-threatening)
- A feeling of insufficient bowel evacuation
Crohn’s disease can cause life-threatening complications in the worst cases. Tears in the anus lining, known as fissures, commonly cause discomfort and blood in stool. Inflammation can cause the intestine to form a fistula, an abnormal channel leading to another part of the large or small intestine, bladder, vagina, or skin.
Other Symptoms
Some people with Crohn’s disease may experience non-gastrointestinal (GI) symptoms that harm their health and quality of life.
- Mouth ulcers
- Painful and swollen joints
- Kidney stones
- Skin problems, such as bumps, sores, and rashes.
- Fever
- Loss of hunger
- Night perspiration
- Weight loss
- Osteoporosis
- Cirrhosis and primary sclerosing cholangitis
- Fatigue
- Eye redness or pain
- Ocular inflammation
- Absence of a regular menstrual cycle
Causes of Crohn’s Disease
The cause of Crohn’s disease is a mystery. The following increase one’s likelihood of developing the condition:
Genetic Variables
If someone with a close relative has Crohn’s disease, family members are more likely to develop the disease. According to studies, 5% to 20% of people with IBD have a parent, child, or sibling with one of the diseases. Crohn’s disease carries a greater genetic risk than ulcerative colitis.
Inflammatory Bowel Disease
Harmful bacteria in the gut may trigger an immune response against healthy tissue by activating different types of antibodies. The inflammation resulting from the immune response is persistent, leading to Crohn’s disease symptoms, including chronic inflammation, ulceration, and intestinal wall thickening.
Environmental Factors
Living conditions appear to influence the development of Crohn’s disease. People living in developed countries suffer more than those in developing countries. Also, urban citizens have more prevalence than people in rural areas.
Smoking
The chance of developing Crohn’s disease may increase by as much as 50% if someone smokes cigarettes. Also, smoking increases the severity of sickness and the likelihood of requiring surgery.
What is Ulcerative Colitis?
Colitis ulcerative (UC) is an inflammatory bowel disease (IBD). IBD is a collection of conditions affecting the gastrointestinal (GI) tract. When the lining of the large intestine (also known as the colon), the rectum, or both become inflamed, UC occurs. This inflammation results in the formation of ulcers on the colon lining.
Typically, inflammation starts in the rectum and spreads upward. It can affect the entire colon. Ulcerative colitis is a chronic disease or condition with profound emotional and social effects on patients.
Symptoms of Ulcerative Colitis
The severity of UC symptoms varies from one individual to another. Signs are also subject to change over time. Individuals with a diagnosis of UC may experience periods of mild or no symptoms.
Common Symptoms
- Rectal discomfort
- Malnutrition and weight loss
- Blood or pus in the stools
- Back pain
- Obesity malnutrition
- Stomach ache
- Higher abdominal noises
Other Symptoms
- Sickness and fatigue
- Diminished appetite
- Skin issues
- Eye inflammation
- Sore throat
- Swollen joints
Causes of Ulcerative Colitis
Eating habits and stress were once thought to be to blame. However, current knowledge suggests that while these may exacerbate ulcerative colitis, they do not cause it.
The following risk factors may contribute to determining which people get UC:
Genes
The risk of developing UC may increase if you inherit a gene from a parent with the disease. Having a close relative with ulcerative colitis also increases your risk of developing the disease, suggesting a genetic component.
Variant Autoimmune Diseases
The risk of developing a double immunological illness increases if you already have one. Thus, you may have UC if you suffer from an immunological disease or disorder already.
The External Environmental Factors
Ulcerative colitis may arise from external factors that enter the body to produce disease. You can get an immune response from antigens and pathogens leading to UC.
Similarities between Crohn’s Disease and Ulcerative Colitis
- These diseases usually develop in teens and young adults but can develop at any age.
- Both have similar symptoms.
- There is no gender difference in the prevalence of both diseases.
- They have similar environmental, genetic, and immune system contributing factors.
Difference Between Crohn’s Disease and Ulcerative Colitis
Definition
Crohn’s Disease
Chronic inflammation of the digestive tract is the hallmark of Crohn’s disease; a kind of inflammatory bowel disease (IBD).
Ulcerative Colitis
Ulcerative colitis, at the same time, also belongs to the IBD category. Ulcerative colitis is a chronic condition that exclusively affects the colon.
Area of Inflammation
Crohn’s Disease
Crohn’s disease can affect any part of the digestive tract from the mouth to the anal canal. Crohn’s disease causes intermittent inflammation around healthy tissue.
Ulcerative Colitis
Ulcerative colitis, on the contrary, only affects the colon. Ulcerative colitis causes continuous inflammation along the entire colon.
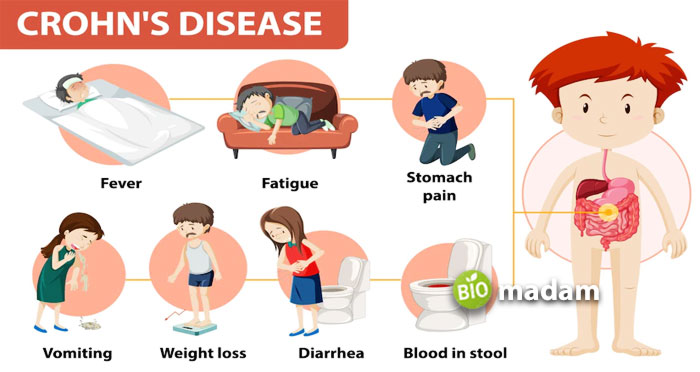
Classification
Crohn’s Disease
Crohn’s disease has the following types depending on the inflammatory area: Ileitis, gastroduodenal, jejunoileitis, and ileocolitis.
Ulcerative Colitis
Ulcerative colitis is categorized into ulcerative proctitis, proctosigmoiditis, left-sided colitis, and pancolitis depending on the location.
Symptoms
Crohn’s Disease
Symptoms of Crohn’s disease include diarrhea, fever, fatigue, abdominal pain, blood in stools, mouth sores, and fistula formation.
Ulcerative Colitis
Malnutrition, weight loss, blood in stools, back pain, higher abdominal noises, sickness, skin issues, diminished appetite, sore throat, and swollen joints are symptoms of ulcerative colitis.
Causes
Crohn’s Disease
Common causes of Crohn’s disease include genetic variables, environmental factors, smoking, and IBD.
Ulcerative Colitis
Similarly, genetics, autoimmune reactions, and external factors like bacteria and viruses may contribute to ulcerative colitis.
Diagnosis
Crohn’s Disease
Diagnosing Crohn’s disease requires two endoscopies. Colonoscopy examines the anus, and upper endoscopy examines the mouth, down the esophagus, into the stomach, and the small intestine to check its functioning.
Ulcerative Colitis
Diagnosing ulcerative colitis requires endoscope insertion through the anus only. Sigmoidoscopy examines the rectum and lower intestine for inflammation. A total colonoscopy checks the whole colon.
Treatment
Crohn’s Disease
Combining dietary changes and medicines is best for treating Crohn’s disease. However, the process of surgery is rare.
Ulcerative Colitis
In contrast, a combination of nutritional changes and drugs is best to treat ulcerative colitis. Here, the procedure of surgery is common.
The Bottom Line
Crohn’s disease and ulcerative colitis are diseases of the gastrointestinal tract. They may arise from underlying infections or diseases; however, genetics play a major role. A fundamental difference between Crohn’s disease and ulcerative colitis is that Crohn’s disease affects the whole GI system. On the other hand, ulcerative colitis leads to colon inflammation. They can be treated through dietary changes. Surgery is also common for ulcerative colitis.
FAQs
Can ulcerative colitis turn into Crohn’s disease?
There have not been many clinical presentations of Ulcerative Colitis patients progressing into Crohn’s Disease. However, a 61-year-old man who underwent colectomy for Ulcerative colitis was then diagnosed with Crohn’s Disease.
Do you look different with Crohn’s disease?
People with Crohn’s Disease may have skin tags or rashes, impacting their appearance. Skin tags can be like moles, pink, flesh-colored, or darker than your skin.
What is the life expectancy of someone with Crohn’s disease and ulcerative colitis?
Crohn’s disease is not deadly if you manage the symptoms and control your diet to avoid disease progression. So, you can expect to live 75 to 78 years, even if you have Crohn’s disease.
What color is poop with Crohn’s?
People with Crohn’s Disease may have red or black stool due to the presence of blood. At the same time, mucus will look yellowish or white in feces.

Jeannie has achieved her Master’s degree in science and technology and is further pursuing a Ph.D. She desires to provide you the validated knowledge about science, technology, and the environment through writing articles.