Macro and micronutrients help your body stay in shape and facilitate body processes. Calcium is one such important nutrient that contributes to bone development and strengthening. However, your body does not absorb calcium the same way in old age leading to loss of bone strength. Furthermore, some factors may also lead to joint inflammation in men and women. These factors also contribute to different bone issues and it can be difficult to differentiate the conditions.
Keep reading to know all the differences between rheumatoid arthritis and osteoporosis.
Comparison Table
| Factors | Rheumatoid Arthritis | Osteoporosis |
| Definition | Joint swelling | Bone weakening |
| Prevalence | 1.5 million | 10 million |
| Symptoms | Swollen, painful joints | Brittle bones, quick fractures |
| Causes | Autoimmune attack | Lack of calcium in bones |
| Risk Factors | Women, age > 45, family history, smoking | Anorexia nervosa, low-calcium |
| Diagnosis | RF test, CBC, CRP, Anti-CCP antibodies | X-rays, MRI, BMD test using DXA |
| Treatment | DMARDs and biological agents | SERMs, parathyroid hormone, Vit. D and calcium supplements |
| Surgery | Joint replacement surgery | Vertebroplasty, Kyphoplasty |
| Complications | Diabetes, heart disease, disability, premature death | Fracture, deformities, bone cancer, heart failure |
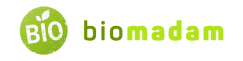
What is Rheumatoid Arthritis?
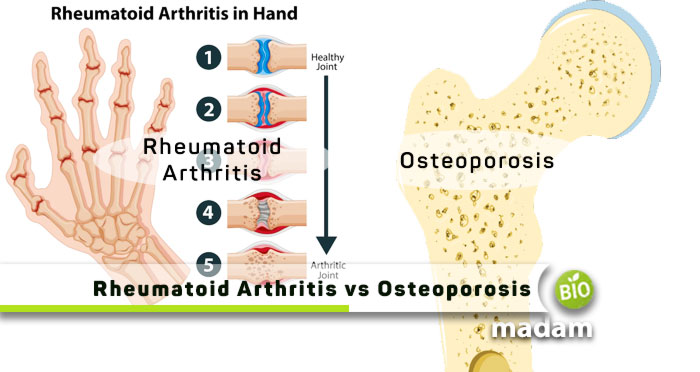
Just like the psoriatic arthritis, rheumatoid arthritis is also an inflammatory disorder causing inflamed joints. Sometimes, it may also affect other body parts besides joints, including the lungs, heart, skin, eyes, or blood vessels. It is an autoimmune disorder which means that the body’s immune system attacks your body tissues.
Rheumatoid arthritis affects 1.3 million adults in America, and the number of women is higher than men.
The unwanted inflammation in rheumatoid arthritis causes the joints to lose their position when the inflammation goes down. Thus, it causes instability in joints and may lead to deformity.
Symptoms of Rheumatoid Arthritis
The most common symptoms of rheumatoid arthritis include the following:
- Inflamed joints
- Stiffness in joints which is usually more severe early morning
- Fever and fatigue
With the passage of time, you may also experience inflammation in elbows, ankles, knees, hips, and shoulders, besides knuckles and wrist joints. Moreover, joints, some people also get swelling in salivary glands, nerve tissues, lungs, skin, bone marrow, and blood vessels.
Causes of Rheumatoid Arthritis
The exact cause of rheumatoid arthritis is not known. However, it results from an autoimmune reaction when the body’s immune system attacks healthy body tissues. Your immune system mistakenly sends antibodies to attack the lining of your joints. Eventually, it damages the surrounding tissues, including cartilage, bones, tendons, and ligaments.
Risk Factors for Rheumatoid Arthritis
Besides the autoimmune reaction, a few factors may put you at a higher risk of rheumatoid arthritis. These include:
- Genetic factors
- Hormones
- Smoking
Yes, it might seem surprising, but researchers have found an increased risk of rheumatoid arthritis in people who smoke frequently. Furthermore, some studies also show that it may run in families and pass down through generations. So, you may be at high risk of rheumatoid arthritis if your immediate family has it. Reports also show that females are 2 to 3 times more susceptible to rheumatoid arthritis than males.
Diagnosis of Rheumatoid Arthritis
The first step in diagnosing rheumatoid arthritis is to visit a general physician. The general physician (GP) will examine your joints to see if they are swollen. Telling the GP all your symptoms will help them discover the exact issue.
Your doctor may ask you for a few test reports to confirm the presence of rheumatoid arthritis. The tests do not directly indicate arthritis, but the test results may confirm the signs and symptoms. The tests include:
- CBC (Complete Blood Count)
- CRP (C-reactive protein) to measure the levels of inflammation
- ESR (Erythrocyte Sedimentation Rate) to assess inflammation levels
- Anti-CCP antibodies to find rheumatoid factors in the blood and plasma
- Joint scans, including MRI and X-rays, to check the condition of the joints
Treatment of Rheumatoid Arthritis
Treatment of rheumatoid arthritis includes using DMARDs (disease-modifying anti-rheumatic drugs) that slow down the progression of the disease or chronic condition. Commonly used drugs are methotrexate, leflunomide, hydroxychloroquine, and sulfasalazine.
With technological advancements, healthcare providers opt for biological treatments in case DMARDs do not help. Adalimumab, etanercept, and infliximab are biological treatments for rheumatoid arthritis (RA).
Moreover, the physician also prescribes medication to relieve pain, like NSAIDs, painkillers, and steroids. RA patients may require physiotherapy and occupational therapy to improve symptoms.
What is Osteoporosis?
The word osteoporosis translates to ‘porous bones.’ Osteoporosis affects the compact and spongy bone in the body. The bones become less dense, and large spaces form between the bony structure, giving it a porous appearance.
Around 10 million people in America have osteoporosis, while 44 million have low bone density. It puts half of the adult American population at risk of osteoporosis, causing easy fractures.
Our body replaces old bones with new ones to avoid anatomical and physiological movement issues. However, the bone mass does not increase when we grow old, escalating the chances of bone breaking. Bones of the wrists, hips, and spine are at a higher risk of breakage in osteoporosis. It is a silent disease that you may not know about until you experience a fracture.

Symptoms of Osteoporosis
As mentioned, osteoporosis does not exhibit any specific symptoms until you break a bone or lose your height over time. These symptoms occur when your bones have been weakened by osteoporosis. Some common indications of osteoporosis may include the following:
- Quick fractures
- Back pain due to collapsed vertebrae
- Stooped posture or loss of height
Causes of Osteoporosis
The primary cause of osteoporosis is natural causes as almost all people get osteoporosis in their old age. However, nutritional factors play a major role in the onset of osteoporosis. People who consume calcium-rich diets like milk, eggs, water chestnuts, and dragon fruits may reduce their risk of osteoporosis.
Risk Factors of Osteoporosis
Some risk factors of osteoporosis besides age and less calcium intake include:
- Physical inactivity or a sedentary lifestyle
- Family history of osteoporosis
- Early menopause
- Hysterectomy before menopause
- Smoking
- Specific medication
Diagnosis of Osteoporosis
Regular screening tests for women are advised to rule out osteoporosis if it develops early. You must report any sudden changes in height, weight, posture, or balance to your general physician. The GP may also check your muscle strength to diagnose osteoporosis.
A few diagnostic tests that help understand the diagnosis and prognosis of osteoporosis include BMD (Bone Mineral Density). Most doctors use dual-energy X-ray absorptiometry (DXA) to determine bone mineral density.
Treatment of Osteoporosis
Osteoporosis is not reversible or curable. However, you can reduce your risks of fractures or bone damage by taking a few measures, like:
- Lifestyle changes
- Exercise
- Avoiding falls
- Calcium and vitamin D intake
- Proper nutrition, including carbs, proteins, and fats
Medicines like bisphosphonates, selective estrogen receptor modulators (SERMs), and parathyroid hormones help maintain bone mass density.
Differences between Rheumatoid Arthritis and Osteoporosis
Definition
Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disease that causes inflammation in joints.
Osteoporosis
On the other hand, osteoporosis refers to the formation of pores in bones in old age.
Prevalence
Rheumatoid Arthritis
24% of all adults in the US have rheumatoid arthritis.
Osteoporosis
Contrarily, around 10 million Americans have osteoporosis, with around half the adult population at risk because of low bone density.
Symptoms
Rheumatoid Arthritis
Symptoms of rheumatoid arthritis include swelling and pain in joints, stiffness of joints, and fever.
Osteoporosis
At the same time, osteoporosis does not exhibit any specific symptoms and is typically understood when a bone breaks.
Causes
Rheumatoid Arthritis
Rheumatoid arthritis results from an autoimmune reaction in the body when different antibodies attack healthy body cells.
Osteoporosis
However, osteoporosis is common in older people as the bones weaken with age. A diet low in calcium also contributes to osteoporosis.
Risk Factors
Rheumatoid Arthritis
Rheumatoid arthritis is more prevalent in women. Thus, women over 45 years of age are at higher risk. Smoking and family history are also additional risk factors.
Osteoporosis
On the contrary, risk factors for osteoporosis include extended medication use, poor lifestyle, fluctuation in sex hormones, and anorexia nervosa.
Diagnosis
Rheumatoid Arthritis
The diagnostic tests for rheumatoid arthritis include the rheumatoid factor (RF) test, CBC, CRP (C-reactive protein), ESR, and anti-CCP antibodies test.
Osteoporosis
Alternatively, physicians use dual-energy X-ray absorptiometry (DXA) to assess the patient’s bone mineral density.
Treatment
Rheumatoid Arthritis
Treatment of rheumatoid arthritis includes DMARDs like methotrexate, leflunomide, hydroxychloroquine, and sulfasalazine. Biological treatment may also help in rheumatoid arthritis.
Osteoporosis
Whereas, osteoporosis treatment involves the use of bisphosphonates, SERMs, and parathyroid hormones. Intake of vitamin D and calcium also improves bone health.
Surgery
Rheumatoid Arthritis
Sometimes patients with rheumatoid arthritis may require joint replacement surgery for knee, hip, or shoulder joints.
Osteoporosis
Conversely, invasive procedures, including vertebroplasty and kyphoplasty, use thin tubes to inject bone cement into affected vertebrae.
Complication
Rheumatoid Arthritis
Untreated rheumatoid arthritis may lead to physical and social consequences like disability, diabetes, premature heart disease, and premature death.
Osteoporosis
In contrast, osteoporosis may worsen and cause fractures, sprains, deformities, osteoarthritis due to stress on bones, bone cancer, or heart failure.
The Bottom Line
Rheumatoid arthritis and osteoporosis are bone and joint-related issues. Often confused with osteoarthritis, rheumatoid arthritis, and osteoporosis are different health problems. They are common in old age but may develop sooner depending on your lifestyle and nutrition intake. Rheumatoid arthritis is an autoimmune inflammatory disorder in which your immune system attacks its joint cells and tissues. On the other hand, osteoporosis arises from a lack of calcium, forming pores in your bones and weakening them. These health conditions can be managed through adequate treatment and prevention of further damage.

Anna has completed her degree in Pharmacy from the University of Hawaii. She is serving as a research assistant in a pharmaceutical company. She had a great interest in writing blogs, traveling to different parts of the US, and trying delicious recipes in her spare time.